Coronavirus (COVID-19): What a Pediatrician Wants You to Know
Elisa Song, MD
healthykidshappykids.com
Flu hysteria has now transformed into coronavirus hysteria, and many of you have asked me how worried you should really be. News around COVID-19 has taken the world by storm and those of us outside of China are not sure whether to panic or stay calm. Addressing the Munich Security Conference on Feb 15, 2020, World Health Organization (WHO) Director-General Dr Tedros Adhanom Ghebreyesus said:
… we’re not just fighting an epidemic; we’re fighting an infodemic …
This is a time for facts, not fear.
This is a time for rationality, not rumours. (1)
I always say that knowledge is power, but in this case, because the world has never seen this particular coronavirus (which is why it’s called “novel”), we don’t know a whole lot. Scientists and researchers across the world are scrambling to learn more about COVID-19 and possible treatment and prevention strategies, and we are learning more everyday. I have to admit that I’m more worried about COVID-19 than I was when Kenzi had the flu with a 105.5 fever. But when I get anxious about something, I try to dig in and get the facts. And that’s what I did – for days. So let me share with you the facts that I’ve uncovered so that we can all be calmly and rationally prepared for a COVID-19 pandemic if it occurs. What follows below is the most evidence-based research I could find to help us navigate these times with as much knowledge as possible. All references are at the end, and I will update as new developments arise. Be forewarned – this is a long article, but I wanted you to have all the information you need in one place, instead of the gazillions of sites and resources I ended up scouring and piecing together.
Let’s fight fear with FACTS!
What is COVID-19?
COVI-19 was first reported in Wuhan, China on December 31, 2019, which started out as an outbreak, has since become an epidemic, and may be set to become a pandemic.
Let’s clarify the terminology. An outbreak happens when a disease occurs in greater numbers than expected in a community, and can even be just one case. You can have outbreaks in different communities. An epidemic is an outbreak that spreads rapidly to many people. A pandemic is an epidemic of global proportions that has become widespread across several countries or continents.
COVID-19 is the name of the respiratory illness caused by the 2019 novel coronavirus that was first detected in Wuhan, China. You will also see it referred to as the 2019 Novel Coronavirus, 2019-nCoV, or SARS-coV-2. Coronaviruses are a large family of viruses that are named for the spikes on their surface that look like crowns (“corona” in Latin means crown). By now, I’m sure you’ve figured out that COVID-19 has nothing to do with the Corona beer that you may have enjoyed at some point with a lime wedge, although many people have searched Google for “Corona beer virus”. Coronaviruses can cause mild illness like the common cold, or more severe illness like we’ve seen with SARS (Severe Acute Respiratory Syndrome) or MERS (Middle East Respiratory Syndrome), and now COVID-19.
How many people actually have COVID-19?
The number of COVID-19 cases and deaths are increasing everyday, so these numbers are a moving target. WHO COVID-19 Situation Reports (2) provide daily reports of worldwide numbers.
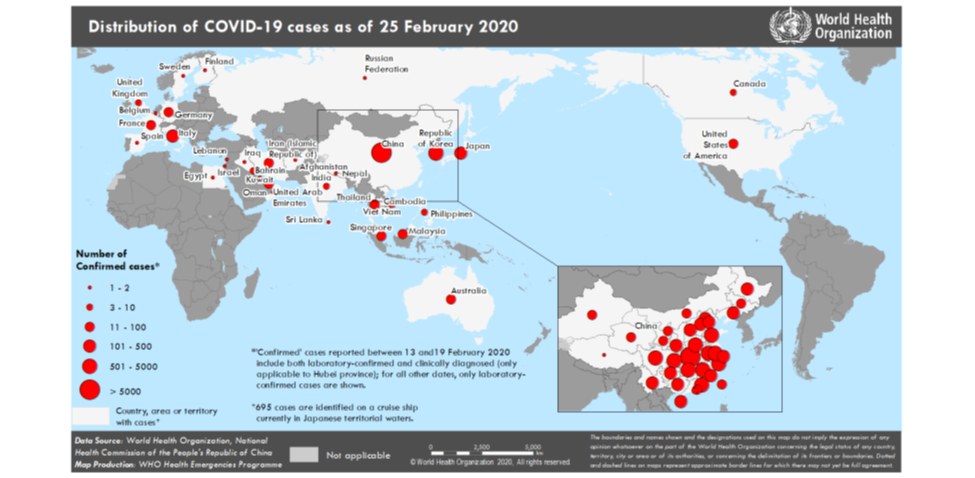
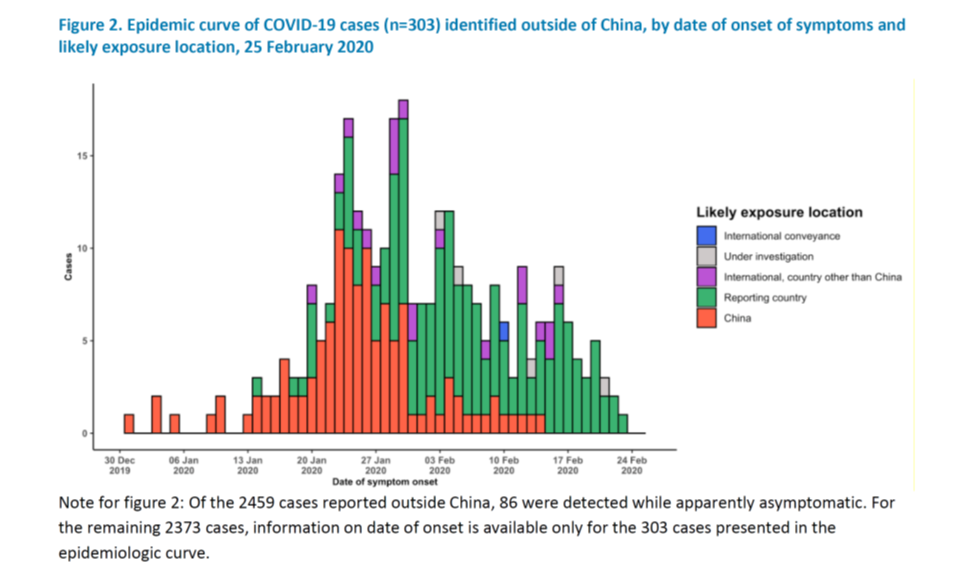
As of February 25, 2020. 88.5% of worldwide COVID-19 cases were still in China, with a reported 77.780 cases. There were 53 cases in the US (with 18 new cases reported that day) – 14 have been traced back to exposure in China, 36 to exposure from an outside country not China, and 2 with domestic exposure. There were a total number of 2,459 cases outside of China (with 390 new cases that day). Of these 2,459 cases, 981 contracted COVID-19 in the reporting country with no personal history of travel to China.
This WHO graph shows that currently, infection from exposure to COVID-19 from within the reporting country is far surpassing infection from exposure due to travel from China or another country. Domestic spread is becoming an increasing concern, and we need to have more strategies for early detection, containment and treatment than just closing our borders. On February 26, the CDC announced the first US case of a man in Solano County in Northern California who has contracted COVID-19 without any history of travel outside the US or close contact with another patient with known infection.
How is COVID-19 transmitted?
It is now clear that human-to-human transmission of COVID-19 is possible and is occurring. Transmission is mainly through respiratory droplets and close contact – similar to how influenza is spread. The CDC defines close contact as being within 6 feet or within a room or care area for a prolonged period without personal protective equipment OR having direct contact with secretions of a person with COVID-19 infection. There is some evidence that fecal-oral or blood transmission may be possible, even when COVID-19 is not detected in oral swabs (3). Investigation is underway to determine how long COVID-19 can survive on various surfaces and possibly be transmitted through “fomites” (a fancy word for objects or materials that can carry infection, such as tabletops, keyboards, clothes and utensils).
The incubation period is thought to be 2-14 days, with a median incubation period of 4 days. Patients are thought to be most contagious when they are symptomatic. However, a recent report (4) found that an asymptomatic woman who transmitted COVID-19 to 5 other people may have had an incubation time of 19 days.
What are the symptoms of COVID-19?
What is important to remember is that the majority of infected people appear to have mild infections – with mild cold-like symptoms and fever, and likely many who have no symptoms. As noted above, there are case reports of asymptomatic carriers. However, most people who contract COVID-19 do seem to develop symptoms of some sort.
Reported symptoms include:
- Fever (which may not be present in the very young or very old, or immunocompromised)
- Uncomplicated upper respiratory symptoms (Cough, sore throat, nasal congestion, malaise, headache, muscle aches)
- Difficulty breathing
- Mild pneumonia
- Severe pneumonia (the severe pneumonia caused by COVID-19 is now named severe acute respiratory infection (SARI))
- Acute Respiratory Distress Syndrome (ARDS)
- Sepsis and Septic shock
- Death
Death is of course what we are all worried about. So let’s look at that a little more closely in the next section.
What is interesting to note is that children seem less vulnerable to infection and appear to have milder symptoms than adults. There have been NO reported deaths in children 0-9 years of age. One very small study of 9 infants under 1 year of age infected with COVID-19 found that none of the infants had severe illness or complications. In fact, 1 had no symptoms, 2 had mild upper respiratory tract symptoms, and 4 had fever. (5)
Pregnant women also do not appear to be at greater risk for complications. In a small study of 9 women in Wuhan in their 3rd trimester of pregnancy with confirmed and symptomatic COVID-19 infection, none developed severe pneumonia or died. All gave birth via c-section to healthy-appearing babies with normal Apgar scores. No virus was found in amniotic fluid, cord blood or breastmilk. (6)
What is the COVID-19 mortality rate?
Unfortunately, we don’t really know. The high number of deaths in China is devastating, but may not be reflective of mortality rates in other parts of the world given the tragic lack of hospital staff, medical supplies, ICU beds, and test kits that China is facing. If we look at the WHO numbers as of February 22, 2020, of the 76,392 reported cases in China, there have been 2348 deaths, which puts the mortality rate in China at 3%. Outside of China, however, there have been 11 deaths out of the 1,402 cases, which is a 0.78% mortality rate.
Certain populations seem to be more at risk for infection and for death. Increasing age seems to be the most important factor, and as mentioned above, children appear relatively spared. In a report released by the Chinese CCDC on February 17, 2020 in the Chinese Journal of Epidemiology, the risk of death increases with age, with being over 80 the highest risk factor. The fatality rate of patients over 80 years old was estimated to be 14.8%. Death in those under 50 appears to be unlikely, with the mortality rate of 40-49 year olds estimated to be 0.4% and 0.2% for patients 10-39 years of age. As noted above, there have been NO deaths in children 0-9 years old. Having a chronic, pre-existing medical condition also significantly increased the risk of death. Without any pre-existing condition, the mortality rate was 0.9%. A history of cardiovascular disease increased the risk to 10.5%. (7)
So like the influenza virus, the elderly and those with underlying chronic medical conditions appear to be most at risk for serious complications and death from COVID-19. However, unlike influenza, children so far appear to be relatively protected.
How and who do you test for COVID-19?
COVID-19 is detected by testing nasopharyngeal swabs (basically a q-tip up the nose), oropharyngeal swabs (a throat swab), and sputum for genetic material of COVID-19 by polymerase chain testing (PCR). The test kit is called the “Centers for Disease Control and Prevention (CDC) 2019-Novel Coronavirus (2019-nCoV) Real-Time Reverse Transcriptase (RT)-PCR Diagnostic Panel.” In the US, these test kits are NOT available currently through doctor’s offices, community clinics, or hospitals (i.e. I do NOT have test kits). If I were suspicious that a child or parent in my office could have COVID-19, I would send them to the public health department for testing.
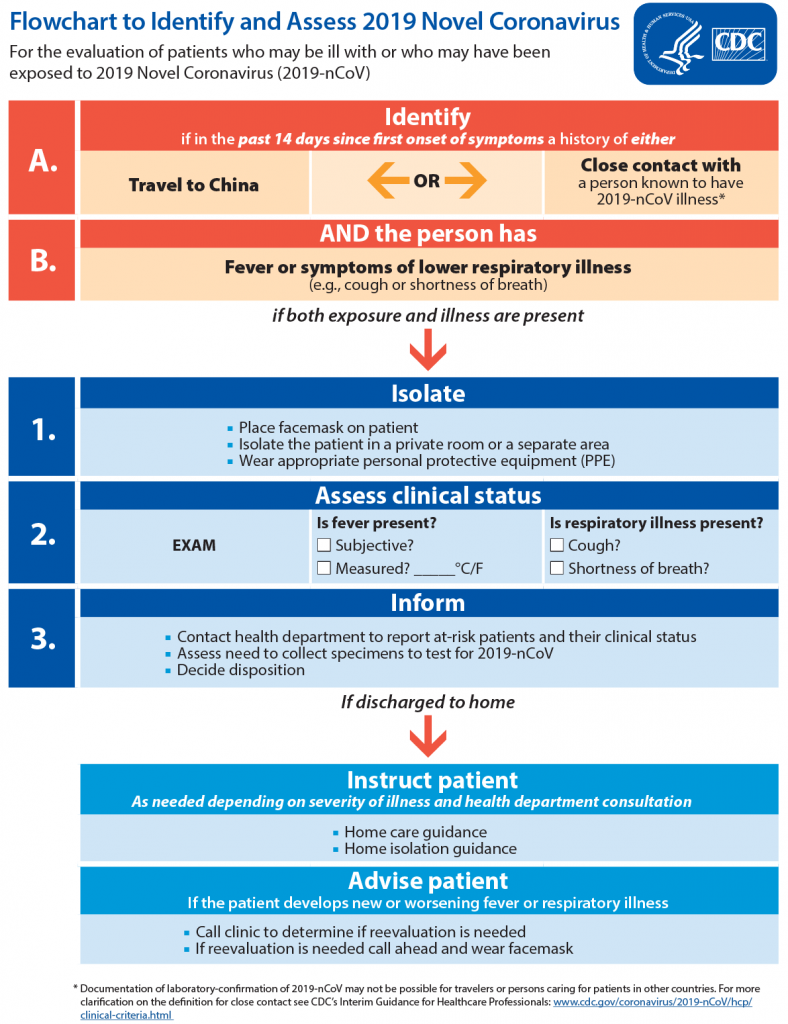
Currently, the recommendations are to test patients with fever and lower respiratory symptoms (cough or shortness of breath) who have traveled from Wuhan, China within 14 days of symptoms onset or have had close contact with a person with confirmed COVID-19. Since the travel ban to and from China was enforced on February 3, we are outside that window for China travel, so I would only consider testing a child with close contact with someone with COVID-19. Remember, the CDC defines close contact as being within 6 feet or within a room or care area for a prolonged period without personal protective equipment OR having direct contact with secretions of a person with COVID-19 infection.
This is the protocol that was emailed to me by my local health department (8):
The CDC also recommends that providers test for other respiratory pathogens, like they would as part of their usual workup for anyone who comes in with fever, runny nose, and cough – like the flu! Because let’s face it, we’re still in the middle of flu season, and …
If you or your child have cold or flu symptoms,
chances are that you have a cold or the flu!
Should we begin to see more domestic spread of COVID-19 in the United States, please …
Do NOT rush to your doctor’s office or hospital to get tested at the first sign of fever or cough unless your health is declining and you need urgent medical attention.
Your doctor or emergency department does not currently have the capability to test for COVID-19, and going unnecessarily to the doctor’s office or emergency department may inadvertently expose you or your child to COVID-19 or other infections and likewise expose other people to whatever illness you may have. Many cases of COVID-19 in China are likely due to uninfected people becoming infected after exposure while waiting in long hospital and clinic lines to be tested.
How do you treat COVID-19?
There are currently no specific antiviral medications known to treat COVID-19, Treatment is supportive with rest, fluids, oxygen, and more intensive care if needed. Scientists are actively researching possible existing or new antiviral medications that may have activity against COVID-19, and vaccines that may help to prevent COVID-19. Tamiflu will not work. While these efforts are critically needed, the manufacture and testing of a new pharmaceutical agents or vaccines is likely several months to over a year in coming.
In the meantime, are there any existing natural treatments that might work? We just don’t know. A huge amount of funding has been committed to clinical treatment trials. While we wait anxiously for results, I urge scientists and researchers to consider some of the evidence we currently have about natural treatments for prior coronavirus outbreaks (SARS, MERS) and sepsis that may theoretically hold promise for successfully treating COVID-19, and would be more readily available and much less costly than any newly-engineered drug.
I am here to educate and inform, NOT to recommend any particular treatments because we simply do not yet know what will be effective against COVID-19. I did this research out of an effort to educate myself on all possible therapeutic options if/when COVID-19 arrives. Here is what I found. These are theoretical possibilities only. Please do not stockpile these natural medicines. If you suspect you or your child has COVID-19, please consult with your physician on your best treatment options.
Sambucus Formosana Nakai (a species of elderberry similar to Sambucus nigra or black elderberry that has been found to have anti-influenza activity) was found to have strong activity against Human coronavirus NL63 (HCoV-NL63). (9) NOTE: This is NOT the same as the elderberry syrup you’ll find on shelves, and I am not recommending that you go out and stockpile Sambucus Nigra). The caffeic acid component of Sambucus Formosana Nakai seemed to be responsible for most of the anti-HCoV-NL63 activity, and significantly inhibited replication and blocked attachment of HCoV-NL63. Caffeic acid is actually NOT related to caffeine, but is found in many foods such as coffee, wine, turmeric, basil, thyme, oregano, sage, cabbage, apples, strawberries, cauliflower, radishes, mushrooms, kale, pears, and olive oil. It definitely couldn’t hurt to load up on caffeic acid-rich foods (minus the coffee and wine, perhaps…).
Traditional Chinese Medicines have been met with significant controversy and panic stockpiling when Chinese researchers claimed that a traditional herbal formula (shuanghuanglian made with honeysuckle, Chinese skullcap and forsythia) could inhibit 2019-nCoV in vitro. This was a premature announcement and clinical trials need to be performed. However, if we look to prior research on other coronaviruses, there are studies showing the efficacy of various Chinese herbal agents against other coronaviruses, including SARS-CoV and CHOV-22E9. (10) These herbal medicines include: Bupleurum, Heteromorpha, and Scrophularia scorodonia (11); Lycoris radiata, Artemisia annua, Pyrrosia lingua, and Lindera aggregata (12); Isatis indigotica and Torreya mucifera (13,14,15); and Houttuynia cordata (16) My hope is that researchers take interest in these initial in-vitro results and consider clinical trials that could potentially find a cure in these natural agents.
COVID-19, sepsis & cytokine storm
When patients with COVID-19 die, it is often due to sepsis, in which the immune system goes haywire and overreacts in what is called a “cytokine storm.” Natural agents that are immunomodulatory and immunoregulatory, and bring BALANCE to an overactive immune system, may be one of the best options to support patients with sepsis. Here’s what the literature shows for what may be helpful for critically ill patients with sepsis.. In life-or-death critical situations like sepsis where conventional medicine does not offer significant success, I would urge researchers to consider all potential treatment options for further investigation.
Vitamin C,1.5 grams IV every 6 hours (6 grams total daily), given with hydrocortisone and thiamine was found to significantly decrease mortality and prevent progressive organ failure in patients with sepsis. In fact, patients treated with the vitamin C protocol had an 8.5% death rate compared with 40.4% in the control group! (17) Thankfully, there is currently a research trial underway to investigate vitamin C infusions for the treatment of severe 2019-nCoV infected pneumonia (18) where patients in the treatment group will receive 24 grams of Vitamin C daily for 7 days.
Vitamin D has been called a “pro-survival molecule.” In this review of the literature on Vitamin D and immunity (19), the authors conclude that:
“… vitamin D not only helps the immune system to be dampened during an excessive or chronic reaction (anti-inflammatory potential) but also to rapidly reach its completion or exhaustion, helping innate cells to kill bacteria or viruses. In this sense, vitamin D maintains its pivotal role as a pro-survival molecule.”
Cathelicidin produced by Vitamin D can neutralize LPS (lipopolysaccharides) that are responsible for so much of the damage that we see in sepsis, and also has antimicrobial and immunomodulatory effects. (20) Vitamin D deficiency may actually be considered a risk factor for sepsis and inflammatory disorders, so please ensure that your and your child’s vitamin D levels are optimized as I discuss below in how to protect your child..
Other Natural Agents: This journal article from 2014, Therapeutic interventions in sepsis: current and anticipated pharmacological agents by Shukla P, et al (21), is probably the best article I’ve found on evidence-based yet outside-the-box thinking of potential natural treatment options for sepsis that warrant further investigation. Here are just a few of the fascinating findings:
- Curcumin has been found to inhibit NF-kB – potent activator of inflammation in sepsis. Curcumin was also found to inhibit binding of LPS and suppress the LPS-induced inflammatory response and damage seen in sepsis, while improving survival, in a mouse model of sepsis. (22)
- Quercetin has also been found to inhibit the NF-kB pathway (23), and to improve survival and decrease cellular damage in a mouse model of sepsis (24,25)
- Naringin, a flavonoid found in the skin of citrus fruit, ameliorated LPS-induced sepsis in mice, via the NF-κB pathway, and reduced LPS-induced acute lung injury (26)
- The probiotic Bacillus sp strain LBP32 has extracellular polysaccharides (EPS) that were found to inhibit the LPS-induced release of many pro-inflammatory mediators (such as NO, ROS, IL-6 and TNF-α) by inhibiting the NF-κB pathway. Researchers were able to demonstrate that EPS could greatly improve the outcome of mice with LPS-induced endotoxic shock (27)
- Boswellia (Frankincense) can inhibit LPS-induced inflammation in sepsis. This study (28) found that Casperome® (Casp), an orally bioavailable soy lecithin-based formulation of standardized frankincense extract, was able to ameliorate the systemic effect and multi-organ damage induced by severe systemic inflammation using a mouse model of sepsis.
- Lomatium dissectum is a Native American traditional root that was claimed to have prevented the Washoe Indian tribes from dying during the 1918 influenza pandemic (also called the Spanish flu pandemic). In SARS-CoV sepsis, one of the inflammatory chemokines involved is CXCL10 (29). Poor prognosis with Influenza A is also associated with CXCL10 dysregulation. Lomation dissectum, used by Native Americans in Western US to treat influenza, was found to inhibit CXCL10 secretion by lung cells and may explain why during the 1918 influenza pandemic, L. dissectum was hailed as the cure for influenza and influenza-associated pneumonia. (30)
Is airplane travel safe right now?
As we see more outbreaks in countries outside of China, the CDC has added several countries to its travel advisories. The alerts below are as of February 25, 2020:
- Level 3 (Warning: avoid all nonessential travel) – China and South Korea
- Level 2 (Alert: consider postponing nonessential travel) – Iran, Italy and Japan
- Level 1 (Watch: practice usual precautions – Hong Kong
- Other destinations with community spread: Singapore, Taiwan, Thailand, Vietnam
Travel advisories are a moving target, and as I write, Italy was just added to the list. If you are planning international travel, keep informed with the CDC’s COVID-19 travel advisory page. Whether you choose to travel or cancel any upcoming plans is a completely personal decision, and I cannot recommend you choose one path or another. I personally am limiting international travel for me and my family. While I am lucky to have a busy domestic travel schedule teaching integrative and pediatric functional medicine to other practitioners, if given the choice, I would limit even my domestic travel until we know more. We all have to make whatever decisions we feel most comfortable with for our families, but if you are planning air travel, please read my airplane travel tips and tricks that I list in my blog post How to Have a Healthy, Happy Holiday.
How can you protect your family from COVID-19?
There are commonsense measures to protect yourself from COVID-19 that you should be practicing regardless of whatever virus is circulating at the moment. The only unique recommendation with COVID-19 is to avoid unnecessary contact with non-domesticated animals due to presumed animal-human transmission. Other commonsense measures to protect yourself and prevent spread of illness include:
- Wash hands frequently, especially before eating or touching your face. Washing hands with warm soap and water for at least 30 seconds is the best option. This study found that washing hands even with plain running water without soap was more effective than ethanol-based hand disinfectants at killing the Influenza A virus! (36)
- Avoid touching your eyes, nose, and mouth! Do your best to keep those little fingers away!
- Stay home when you’re sick, unless you need urgent medical attention. You may be increasing your possible exposures to COVID-19 if you don’t have it, or exposing others unnecessarily if you do.
- Cover your cough with your elbow or tissues. Teach your kids proper cough etiquette. And if you use a tissue, immediately throw it into the trash and wash your hands.
- Keep your distance. Try to stay at least 6 feet away from anyone who is obviously sick with fever and/or respiratory symptoms.
- Irrigate your nose. While we do not know if nasal irrigation makes a difference for prevention of COVID-19, I believe that one of the MOST preventive things you can do for any viral respiratory illness is to irrigate your, and your children’s, nasal passages with Xlear nasal spray at the end of every day and after any potential exposure (work, school, playgroups, plane travel, etc.). This is a saline nasal spray with xylitol and grapefruit seed extract, both of which have antimicrobial properties. You cannot overdo it, and will not get “addicted” to it. Other options for nasal irrigation are a regular saline spray, Neti pot, and other sinus rinses like Neilmed.
**Apart from regular hand washing, I believe that daily and frequent nasal irrigation is one of the MOST important things that we can do to prevent influenza and other viral respiratory infections from taking hold.** This is because after exposure to a virus, the influenza virus tries to invade and multiply in your nasal passages for at least 1-2 days before you develop any symptoms. Nasal irrigation can wash away viral particles before they have the opportunity to take hold, and thereby prevent many infections from happening in the first place! - Load up on foods and spices with antiviral properties. These include coconut oil, raw garlic, oregano, ginger, kimchi and other fermented foods, walnut, pomegranate, green tea, apple cider vinegar, and medicinal mushrooms (shiitake, maitake, reishi, cordyceps, turkeytail).
- Eat lots of colorful fruits and vegetables. They are full of antioxidants which will destroy the free radicals that weaken our immune system and are responsible for making us feel sick when we catch a bug. Each color provides different antioxidant power – so be sure to eat a rainbow everyday. If you’re kids aren’t the hugest vegetable eaters yet, give them their antioxidant dose with a smoothie packed with fruits AND veggies, use that smoothie to make jello with grass-fed gelatin or popsicles, sneak pureed vegetables into your spaghtetti sauce, soups, chilis, or whatever other way you can think of – be creative!
- Stay well-hydrated. Stick to water, coconut water, herbal teas, and bone broth. No soda or sugary drinks, please! What’s a good estimate for how much water you need at a minimum? Divide your body weight (in pounds) in half and drink that number in ounces! Do you come close?
- Drink your bone broth! Bone broth has amazing immune-supporting properties. See Amazing Bone Broth to get started easily making your own.
- Eat fermented foods. The probiotics contained in fermented foods have tremendous immune boosting powers. In fact, the fermented Korean cabbage, kimchi, was found to have significant effects in preventing and fighting the H1N1 influenza virus! Other examples of delicious fermented foods to try include sauerkraut, pickles (try “real” pickles without added vinegar like Bubbies), miso, kefir, and kombucha.
- Avoid simple sugars and processed/junk food. Did you know that your blood shows lab evidence of a lowered immune system within 30 minutes of eating simple sugars (like glucose, refined sugar, and fructose), and causes a 50% reduction in your white blood cells’ abilities to kill germs? White blood cells are our “army” cells that fight off germs. This effect is most noticeable 2 hours after ingestion, but is still present 5 hours later! Keeping blood sugar levels healthy has been shown to improve immune system activity.
- Get fresh air and moderate daily exercise. Moderate exercise can boost the production of macrophages, the kind of white blood cells that “eat” bacteria and viruses. However, intense exercise can actually temporarily decrease immune function – so don’t overdo it!
- Get adequate sleep. An increase in sleep actually increases the number of your white blood cells. On the other hand, loss of sleep even for a few hours at night, increases inflammation in our body which makes us more susceptible to catching the flu and having more severe symptoms. So make sure your whole family is getting enough zzzz’s. For tips on getting a good night’s sleep, see Eat Yourself to a Good Night’s Sleep and The 3 Things You Need to Know to Get a Good Night’s Sleep.
- Minimize stress. Emotional stress creates physiological stress in our bodies that lowers our immune defenses and makes us more vulnerable to illness. Stress has been shown to lower our white blood cells’ abilities to kill germs, and actually creates more inflammation that may make us feel even sicker. For guidance on how to help manage your child’s stress naturally, take a look atBack-to-School, Back to … STRESS!!! for some great tips.
Should I wear a mask?
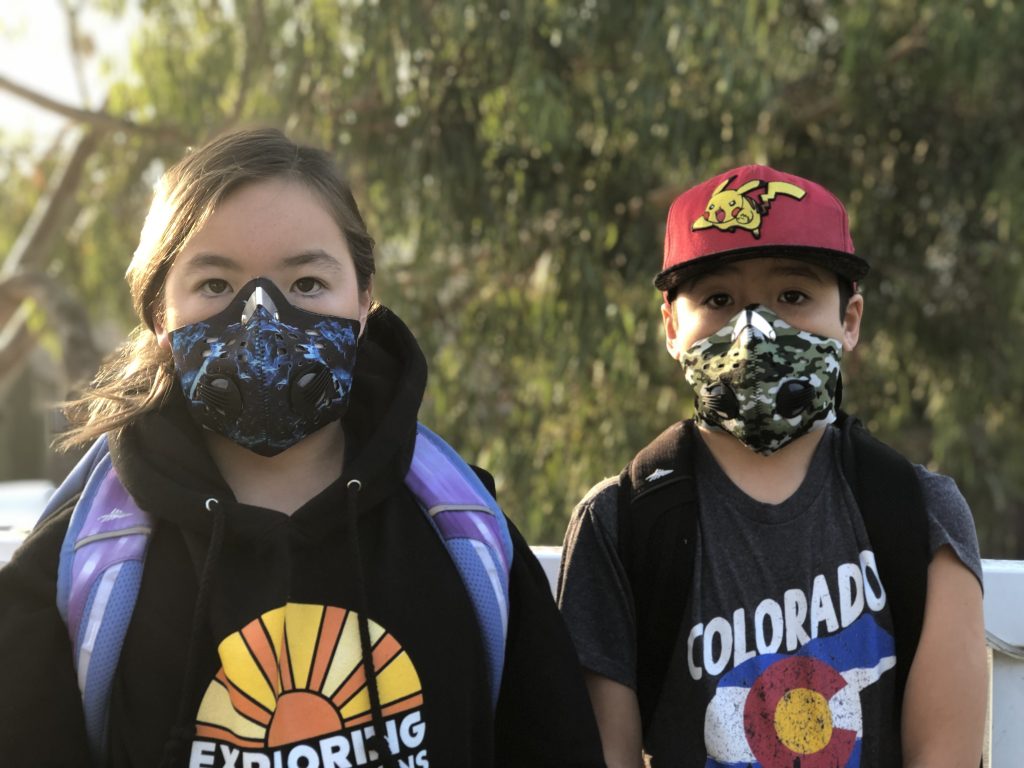
Face masks are currently not recommended for the general public. They are only recommended if you have a cough that you could transmit, or are taking care of someone who is sick with COVID-19.
That being said, this new research paper from February 19, 2020 that has yet to be published (32) compared medical staff at Zhongnan Hospital caring for patients with COVID-19 between Jan 2-22 who were medical staff in the Respiratory, ICU and Infectious Disease Departments and wore N95 respirators and washed hands frequently vs. medical staff in the Hepatobiliary Pancreatic Surgery, Trauma and Microsurgery and Urology Departments who who wore no masks and disinfected their hands less frequently. Even though the masked group actually encountered more confirmed cases of COVID-19 than the unmasked (730% MORE cases, in fact), none of of the 280 staff contracted 2019-nCoV. On the other hand, 10 of the unmasked group became infected.
So, if the pandemic starts to hit a little too close to home, will I be wearing a mask and make Peter, Kenzi and Bodi wear one? Probably yes! If you do wear a face mask, please make sure it’s a “Particulate Respirator Mask” that filters at least 95% of very small particles and is marked P95, R95 or N95, has 2 straps, and forms a tight seal around your nose and mouth. A regular surgical mask will provide no protection and is actually meant to protect others from your cough or sneeze. A properly fitted respirator mask should be worn over BOTH the nose and mouth, and form a tight seal so that you can’t smell any ambient odors. A good test is to put on the mask covering your mouth and nose, pinch the mask across the bridge of your nose, then spray peppermint or lavender essential oil in front of your face. You should not be able to smell or taste any of the oil in your nose or mouth through the mask.
THE PROBLEM: Most masks won’t properly fit and create a good seal over a young child’s mouth and nose to filter out small smoke and air pollution particles, so make sure you follow the suggestions below for immune boosting. Remember, though, that preliminary reports seem to show that children are much more likely to have mild and even asymptomatic disease.
Another problem is that because of COVID-19, N95 masks are currently very difficult to find or are very expensive. Manufacturers should be gearing up their production to fix this problem, so stay on the lookout.
Keep your immune system as strong as possible.
Consider keeping your immune system even more supported with the following nutritional supplements to give your body even more antiviral defense:
- Fish oil – Omega-3 essential fatty acids have a host of immune benefits too long to list!
- Probiotics – One study showed a dramatic reduction in fever and upper respiratory symptoms in children who took a probiotic with a specific combination of Lactobacillus and Bifidobacterium daily throughout the cold and flu season. This particular combination of Lactobacillus and Bifidobacterium can be found in Metagenics Ultra Flora Children’s Chewable probiotic, Ultra Flora Synergy powder, and Ultra Flora Balance capsules. The recommended dosage for children and adults is ¼ tsp 2x/day, 1 capsule 2x/day, or 1 chew 2x/day. Probiotics are why fermented foods pack such a punch, so if your child’s palate hasn’t expanded yet to include a lot of fermented foods, be sure to give her a probiotic supplement to keep her gut and immune system healthy! If you want to know more about which probiotic supplement is right for your child, be sure to download my FREE Guide to Choosing Your Child’s Probiotic!
- Vitamin C – Vitamin C is a powerful antioxidant which assists our ability to ward off and deal with infection. Remember the vitamin C and sepsis study above? I have been using Metagenics Ultra-Potent C because it has added ingredients such as lysine and glutathione which assist in fighting viruses.
- Vitamin D3 – There is speculation that rates of illness increase over the winter because of the widespread deficiency of Vitamin D. As mentioned above, Vitamin D deficiency may be one of the risk factors for sepsis. Studies have shown that people supplemented with adequate levels of Vitamin D3 during the cold and flu season had significantly lower rates of infection. Vitamin D3 increases our body’s production of cathelicidin, an antimicrobial compound, to help fight viral and bacterial infections, that I discussed above in the section on sepsis. The Vitamin D Council recommends a maintenance dosage of 1000IU of Vitamin D3 per 25 pounds of body weight (the dosage may be higher in people with Vitamin D deficiency, which is epidemic and can be measured through an easy blood test). **Vitamin D3 is one of the supplements that I am “religious” about giving to my kids.**
- Zinc – Zinc is required for the normal functioning of white blood cells. Supplementing with just 15mg of zinc per day in adults has been found to improve our immune cells’ ability to ward off infection.
If you or your child does get sick…
If you DO start to feel a fever and cough coming on, remember – it is very likely the common cold, influenza, or one of the other more commonly circulating viruses and NOT COVID-19 – so DON’T PANIC. And even if it is COVID-19, remember that most people appear to have MILD symptoms. If I were concerned that I or my family had COVID-19, I would still use the same pediatrician-approved natural remedies for colds and flu-like illnesses that I detail in these 2 resources:
- My article Pediatrician-Approved Natural Remedies for the Flu
- My online course Everyday Holistic Pediatrics – the ONLY comprehensive online video course of pediatrician-designed, mama-approved natural remedies to boost your child’s immune system and get them through their fever, flu, cold, cough, earache, vomiting/diarrhea, sore throat and pinkeye using diet and lifestyle, homeopathy, herbs, essential oils, and acupressure!
As a disclaimer, I am not in any way recommending natural treatments as a replacement for standard medical care or vaccination, but until that time that effective medical treatments or vaccination for COVID-19 are developed and approved for use in kids and adults, I will be using all the tools I have that I know can work for other viral respiratory illnesses, like the flu. And you bet if Kenzi and Bodi get sick, I will be pulling out my vitamin D3, vitamin C, Windbreaker, Elderberry syrup and VClear, OnGuard or Thieves essential oil, and loading them up with antioxidant-rich foods. For an easy reference, you can download my FREE GUIDE: Natural Remedies to Beat the Flu! (This is for the flu, but may have relevance for COVID-19).
Phew – there you have it. Everything I’ve learned so far and want you to know about COVID-19, and everything I intend to do for my family, from a holistic pediatricians’ perspective. We will continue to learn as more research is done, and I’ll be sure to update this post to share everything I know so make sure you’re signed up for my newsletter to be the first to know of any updates.. In the meantime, stay calm but be prepared.
If you found this useful, please be sure to share with anyone you know who could benefit.
xo Holistic mama doc – Elisa Song, MD
Keep Up to Date on the Latest COVID-19 News:
- WHO: Coronavirus disease (COVID-19) outbreak https://www.who.int/emergencies/diseases/novel-coronavirus-2019
- CDC Coronavirus Disease 2019 page https://www.cdc.gov/coronavirus/2019-ncov/index.html
- WHO COVID-19 Situation Reports: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports
- CDC’s COVD-19 travel advisory page https://www.cdc.gov/coronavirus/2019-ncov/travelers/index.html
References:
- www.who.int/dg/speeches/detail/munich-security-conference
- WHO COVID-19 Situation Reports: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports
- https://www.tandfonline.com/doi/full/10.1080/22221751.2020.1729071
- https://jamanetwork.com/journals/jama/fullarticle/2762028
- https://jamanetwork.com/journals/jama/fullarticle/2761659
- https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)30360-3/fulltext
- http://weekly.chinacdc.cn/en/article/id/e53946e2-c6c4-41e9-9a9b-fea8db1a8f51
- https://www.cdc.gov/coronavirus/2019-ncov/hcp/identify-assess-flowchart.html
- https://www.ncbi.nlm.nih.gov/pubmed/31560964
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4032839/
- https://www.ncbi.nlm.nih.gov/pubmed/16789928
- https://www.ncbi.nlm.nih.gov/pubmed/15885816
- https://www.ncbi.nlm.nih.gov/pubmed/16115693
- https://www.ncbi.nlm.nih.gov/pubmed/20934345
- https://www.ncbi.nlm.nih.gov/pubmed/22578462
- https://www.ncbi.nlm.nih.gov/pubmed/18479853
- https://doi.org/10.1016/j.chest.2016.11.036
- https://clinicaltrials.gov/ct2/show/NCT04264533
- https://www.clinicaltherapeutics.com/article/S0149-2918(17)30235-7/fulltext
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4253453/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4253453/
- https://www.ncbi.nlm.nih.gov/pubmed/17609337
- https://www.ncbi.nlm.nih.gov/pubmed/15668926
- https://www.sciencedirect.com/science/article/abs/pii/S1756464619301203
- https://www.ncbi.nlm.nih.gov/pubmed/31377749
- https://www.ncbi.nlm.nih.gov/pubmed/21640201
- https://www.ncbi.nlm.nih.gov/pubmed/24201081
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5921439/
- https://jvi.asm.org/content/81/1/416
- https://journal.restorativemedicine.org/index.php/journal/article/view/46
- https://msphere.asm.org/content/4/5/e00474-19
- https://www.medrxiv.org/content/10.1101/2020.02.18.20021881v
____
https://healthykidshappykids.com/2020/02/27/coronavirus-covid-19/