Be Still My Beating Kidneys (Part 3 of 3)
Interfering with the Blood Pressure Leads to Kidney Disaster.
Medicine Girl
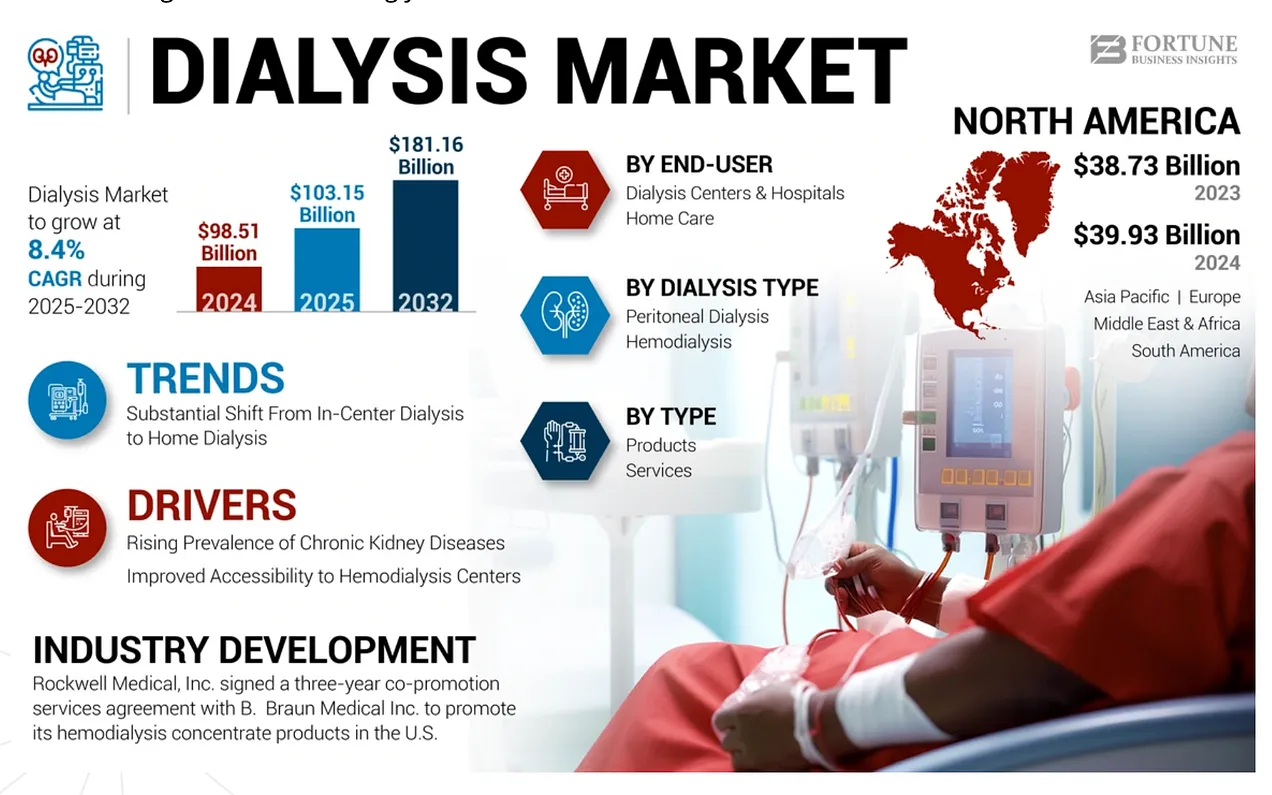
Why the Dialysis Stories Matter
I included stories about dialysis for a reason. Not for shock value or to scare people, but because after nearly four decades working in “medicine”, I occupy a strange position that most people never see from. I don’t just meet patients at the beginning of their diagnosis. I meet them at the end of the road. If you didn’t get a change to read those yet, here you go:

I see people after years and decades of doing what they were told to do. They took the medications. They lowered the numbers. They trusted that controlling blood pressure meant controlling risk. And yet, many of them still arrive at dialysis with bodies swollen with fluid, exhausted hearts, failing kidneys, and a sense of disbelief that this is where everything led. One particular patient always had very high pressures, 180/100, and it was a trick to get them down. When she finally agreed to go to hospice and went off all of her medications, the statin drugs, the 3 blood pressure drugs, the blood thinner, and gabapentin, her pressures were low, 128/84 was the first one, then the subsequent visits were 120/74, 116/59, and stayed there. This happens over and over after they go off the drugs. First, it stays high, and then it drops to “acceptable” levels. Just in time to eke out the last dollar for care before they die.
From one angle, this is a disadvantage. It means witnessing the slow, quiet accumulation of devastation. From another angle, it is an advantage, because patterns become impossible to ignore when you see the long arc instead of isolated moments. You start to recognize that what looks like success early on does not translate into resilience later. And it goes without saying, if I can see it, so can everyone else. The hospice MD laughed about why her 110-year-old patient was suddenly getting better after getting into hospice. “Because we took him off the drugs” lol lol lol “…and now we have to take him off hospice because he is fine” lol lol lol. I don’t find it funny. Not in the slightest.
Dialysis is often treated as an unfortunate but unavoidable outcome, the natural progression of disease. In reality, it represents the point at which the kidneys can no longer perform their most basic function: filtering the blood well enough to sustain life. Reaching that point is rarely sudden. It is usually the result of years of strain, compensation, and missed opportunities to address root causes.
This is why this article goes further than the first two. Those pieces focused on reframing how we think about blood vs kidney pressure and kidney function. This one asks a harder question: what happens when we rely primarily on medications to manage a signal, while leaving diet, movement, stress, and daily habits largely untouched? The idea that there is a pill for every ill is standard operating procedure in ANY medical setting, allopathic or functional.
We Know the Kidneys Are Failing
To understand why kidney function matters so much, we have to be clear about what the kidneys are actually responsible for removing from the body.
Metabolic waste is produced in very specific, ordinary ways. When muscles contract, they burn fuel to create movement, and that process generates byproducts like creatinine. When we eat food, especially protein, the body breaks it down into amino acids to build and repair tissue. What the body cannot use gets converted into nitrogen-based waste, primarily urea. Every heartbeat, every step, every meal adds more of these waste products into the bloodstream, which must be cleared before serious effects begin to develop.
This waste enters the blood because the blood is the transport system. It carries nutrients to cells but also carries away the byproducts of metabolism. As long as we are alive and breathing, waste is continuously dumped into circulation. There is no off switch. The only way to prevent these substances from building up to toxic levels is constant filtration by the kidneys.
The most important metabolic wastes include ammonia and urea from protein metabolism, creatinine from muscle activity, uric acid from the breakdown of genetic material, excess electrolytes like potassium and phosphorus, and acidic compounds that would otherwise alter blood pH. These substances cannot remain in the bloodstream indefinitely or you will die.
We know these wastes exist because we can measure them and do so constantly with dialysis. Blood tests rise when filtration slows. Urine contains them when filtration is working. Urine is not a random fluid loss. It is evidence that the kidneys are functioning properly. Its composition tells us what has been successfully removed from circulation. Which is just one of the smoking guns for why you should NEVER drink urine.
When the kidneys begin to fail, this process breaks down quickly. Waste accumulates. Fluid is retained. Blood volume increases. Fluid leaves blood vessels and enters tissues, causing swelling in the legs, abdomen, and lungs. This is why people with kidney failure look like they are filling up with water. Without adequate filtration, this progression does not take years. People who stop clearing metabolic waste do not slowly decline. They become critically ill within weeks. Dialysis exists for one reason only: to replace kidney filtration when the body can no longer do it on its own and keep the person alive and chained to the for-profit machines.
One of the earliest and most important signs that kidney filtration is impaired is the presence of protein in the urine. Under normal conditions, protein molecules are too large to pass through the kidney’s filtration barrier. When protein appears in the urine, it means that the barrier has been compromised. Proteinuria is not a lab quirk. It is a structural warning. It tells us that the kidney is no longer filtering cleanly and that the system is under strain.
Kidney disease is not diagnosed by a single moment or number. It is recognized through patterns: rising waste markers, protein loss in urine, fluid retention, and declining resilience. These changes reflect a system that is being pushed beyond its capacity to maintain balance.
This is the foundation. Before talking about medications, pressure, or long-term outcomes, it has to be clear what is at stake. The kidneys are not optional accessories. They are the body’s primary defense against internal toxicity. When that defense weakens, everything else follows.
Fixed Kidney Load, Reduced Force
The kidneys do not passively accept whatever blood flow they receive. They require a continuously adjustable pressure range to filter blood effectively, because the amount of waste in the blood is constantly changing.
That pressure is generated by the heart and delivered through the arterial system.
When the heart contracts, it creates the force that pushes blood through the kidney’s filtration units. If that force is reduced, less blood is filtered per unit of time. Filtration slows. Waste begins to accumulate in the bloodstream. The kidneys sense this immediately.
What matters here is not the number on a blood pressure cuff, but the pressure at the level of the kidney filters. Lowering the heart’s ability to generate force lowers filtration pressure unless something else changes to compensate.
So when pressure drops, the kidneys respond by compensating internally.
They adjust resistance within the kidney itself. Blood vessels feeding the filters are narrowed or widened to redirect pressure. Blood flow is redistributed to favor filtration over other functions. Hormonal systems are leaned on more heavily to preserve enough force to keep filtration going.
In the short term, this works. Filtration is preserved. Blood tests may remain stable. There is no immediate failure.
But the workload has not been reduced. It has been shifted.
Instead of being carried by the broader circulatory system, a greater burden is transferred to smaller, more fragile structures within the kidney. Filtration is achieved by squeezing performance out of the system rather than allowing it to operate under relaxed conditions.
Over time, this becomes the default operating state. Chronic UTI’s, kidney stones, more frequent urination, lower flank and back aches can be initial signs of kidney stress.
Structures designed to function across a wide range of pressures are held in a narrowed range. The filters experience higher localized stress even though overall blood pressure appears lower. The system loses flexibility. It becomes less tolerant of dehydration, illness, heat, stress, and changes in medication.
This is why lowering blood pressure is never protective for the kidneys. It depends entirely on whether the underlying load has been reduced.
Blood pressure drugs lower pressure in different ways. Some reduce the force of heart contraction. Some relax blood vessels, so resistance drops. Some reduce circulating volume. Some interfere with signaling systems that normally raise pressure. The details differ, but the outcome is the same: less force is delivered to the kidneys.
What does not change is the amount of waste that must still be filtered.
This is the mismatch.
Blood pressure drugs do not reduce the kidneys’ workload. They reduce the force available to meet that workload. The kidney makes up the difference through chronic internal compensation, which drives long-term damage.
Nothing about this requires the drugs to be toxic. Nothing requires bad intentions. Nothing requires dramatic early failure.
It is simply a system being asked to do the same job under constrained conditions for too long. “Once you understand this mismatch, the next question becomes unavoidable: what increases the load in the first place?”
High-Protein and All-Meat Diets
Protein metabolism produces nitrogen waste, primarily urea. The more protein consumed, the more waste must be filtered. All-meat and very high-protein diets dramatically increase filtration demand. This does not appear as a failure immediately. It shows up as an increased workload year after year.
Influencers promoting all-meat diets rarely talk about kidneys because kidney damage is slow, quiet, and delayed.
Alcohol
Alcohol metabolism generates waste, disrupts fluid balance, and increases vascular resistance. Chronic use keeps the system in a state where higher pressure is required just to maintain baseline function.
Nicotine
Nicotine constricts blood vessels and increases oxidative stress. That increases resistance throughout the circulatory system, making it harder for the heart to deliver adequate pressure to the kidneys.
Caffeine
Caffeine stimulates the nervous system and raises baseline vascular tone. For someone already compensating, this repeatedly pushes the system toward higher demand.
Chronic Stress
Stress hormones tighten blood vessels and alter fluid handling. A chronically stressed body requires higher pressure to move blood through a more resistant system.
Drinking Excess Water
Blindly following government slogans like “drink eight 8-ounce glasses of water a day” is not benign advice, especially for the kidneys. You already have a hydration regulator. It’s called thirst. When it works, it works well.
Healthy kidneys evolved to manage fluid based on need, not based on a schedule or a bottle with time markers. Just like animals in the wild, when you are thirsty, you drink. When you are not, you stop.
Andy Kaufman’s assertion that drinking more water solves the high pressures is wrong-just diluting the problem to lower the pressure is simply cause and effect. In states of increased metabolic load, resistance, or clearance demand, a higher blood pressure is a normal adaptive response that preserves kidney filtration and prevents internal toxicity, not a pathology to be reflexively suppressed.
You haven’t addressed the underlying issues AND you have altered pressure, lowering pressure doesn’t mean improvement. There is plenty of evidence to support healthy higher pressures.
Walking around all day, sipping water from the adult version of a sippy cup, overrides this system. Sure, you look ridiculous, but more importantly, you are forcing your kidneys to do unnecessary work.
Every extra sip has to be filtered, balanced, and excreted. Excess water increases filtration demand, dilutes electrolytes, and forces the kidneys to adjust sodium and water handling to keep blood chemistry stable. In people with already stressed kidneys, this can contribute to fluid overload, swelling, and worsening pressure dynamics. More water does not mean cleaner blood. It often means more kidney labor for no benefit. Yes drinking excess water past your thirst can be detrimental.
“Obey your thirst” is right about one thing: don’t drink unless you are thirsty, and don’t drink anything but water. Juice, soda, sweetened drinks, and “hydration products” only add metabolic load. If salt and lemon water genuinely quenches thirst and tastes like nirvana, fine. But only if it satisfies thirst. Not because you think you’re supposed to be drinking something all the time.
Hydration is not a virtue contest. It is not about hitting a quota. It is about respecting the kidneys’ role in regulating volume. When you drink past thirst, you force the kidneys into constant correction mode. When you listen to them, you let them do what they were designed to do without unnecessary interference.
Put the sippy cup down. Your kidneys will thank you.
Electrolyte Manipulation
Electrolytes are not supplements. They are mechanical and electrical regulators of pressure and flow.
Blood does not move through vessels by force alone. It also moves along electrical gradients. Gerald Pollack’s work and David Parker of What Really Makes You Ill demonstrate that water structured next to biological blood vessel surfaces carries a negative charge, and that this charge separation contributes to blood flow without requiring added pressure.
Blood itself carries a net negative electrical charge when pH and electrolyte balance are intact. Healthy blood vessels also maintain a negative surface charge. When those charges are preserved, blood moves efficiently. Flow is supported, resistance is lower, and less pressure is required to achieve filtration. Disrupt the charge, and the system must rely more heavily on force.
Electrolytes determine the charge environment.
Sodium: Context, Charge, and Consistency Matter
Sodium is required to maintain circulating volume, filtration pressure, and electrical charge balance. Adequate sodium supports blood volume and helps preserve the electrochemical conditions that allow blood to move efficiently.
The problem is not sodium itself.
The problem is how it is delivered and how erratically it is manipulated.
Manufactured sodium chloride delivers sodium as a free charge. It lacks the trace minerals that help stabilize electrical balance and vascular surface charge. Absorption is abrupt. Volume shifts are sharp. Electrical gradients fluctuate.
Sea salt, by contrast, delivers balanced accompanying minerals that support steadier charge balance. It behaves less like a blunt load and more like a physiologic signal.
Chronic low-sodium diets are particularly disruptive. Restriction lowers blood volume and alters charge gradients. Blood becomes harder to move. Resistance rises. The kidneys compensate by increasing internal pressure to preserve filtration.
BP Drugs Disrupt “Potassium”
Potassium is electrically active. It directly controls vascular tone, cardiac conduction, and cellular excitability. Its balance depends almost entirely on adequate kidney filtration and pressure. Many blood pressure drugs disrupt this balance by design.
Diuretics lower pressure by forcing sodium and water out of the body through the kidneys. Potassium is lost alongside them. This is not a random effect; it is the mechanism of action. Blood volume drops, filtration pressure drops, and potassium is excreted in excess.
The result is low potassium levels, which destabilize electrical signaling. Heart rhythm becomes vulnerable. Vessels lose smooth tone control. Pressure regulation becomes erratic instead of adaptive. This is why patients taking B/P drugs often get heart arrhythmias.
Other blood pressure drugs interfere by reducing kidney perfusion or altering hormonal signaling that normally fine-tunes potassium handling. In all cases, potassium control becomes less precise because the kidney is being forced to work under constrained pressure.
Potassium supplements are often added to correct the problem of drug intervention. This assumes intact clearance. When kidney reserve is limited, potassium can swing from low to dangerously high with little warning. Both extremes are dangerous and potentially fatal.
Low potassium increases irritability and arrhythmia risk.
High potassium suppresses conduction and can stop the heart.
By the way, potassium is not a vitamin, and the supplements are not food-derived. They are industrial potassium salts sourced from potash, a mined mineral deposit usually formed from ashes. Potassium is chemically created like a soup and is not a natural element on the Periodic Fable of Elements. It is created by chemically reacting potash with acids or bases to form stable salts that act like potassium chemically in the body, forming compounds such as chloride, citrate, or gluconate. This reaction is required because elemental potassium is extremely reactive and unsafe. The end product is a chemically created and then refined ionic compound designed for stability and absorption, not for physiologic pacing or regulation.
These compounds dissociate rapidly upon ingestion, releasing free potassium into circulation. There is no food matrix, no gradual release, and no buffering context.
This matters because potassium safety depends on the rate and clearance. Food-based potassium arrives slowly and is self-limiting. Supplemental potassium arrives as a chemical bolus (a massive, all-at-once loading dose) and places the full burden of regulation on the kidneys. Boom. That’s the sound of the 57th smoking gun against altering blood pressure in any way, shape, or form.
Calcium and Vitamin D: Charge Loss Through Stiffening
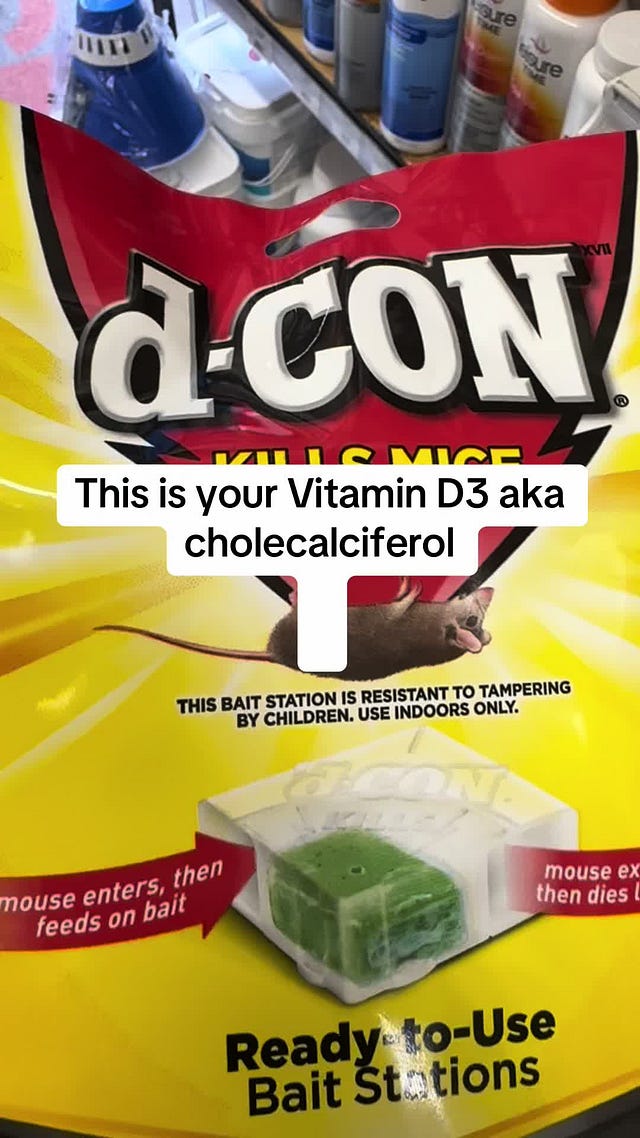
Calcium regulates muscle contraction, including that of the heart and blood vessels. Chronic supplementation, especially when amplified by vitamin D, cholecalciferol, or D-Con Rat poison, promotes calcification and stiffness of all blood vessels AND the glomerular capsules of the kidneys, causing pieces of the filters to break off, also known as kidney stones.
Stiff vessels lose surface charge integrity. Electrical flow becomes less efficient. More pressure is required to move blood through a hardened system.
This is how leaching calcium and other minerals from bone quietly increases pressure demand while appearing “supportive” on paper. The mechanism is not unique to humans. In animals with bones, the same process applies: minerals are pulled from structural tissue into the bloodstream under chronic chemical pressure, raising circulating calcium and gradually calcifying vessels, organs, and filtration surfaces. What starts as redistribution ends as stiffening, and stiff systems require higher pressure to function.
There is no debate here. This is basic biology. When something dissolves bone, it does not magically become health-promoting just because the dose is smaller, the label is nicer, or your hero told you it was beneficial. The fact that it reliably kills small animals should have been the first clue, not the ninety-eighth smoking gun.
Magnesium works because it relaxes muscles and alters electrical gradients.
It relaxes skeletal, vascular smooth, and cardiac muscles. Vascular tone drops. Resistance drops. Electrical signaling shifts. Blood pressure falls. Magnesium’s action is functionally similar to drugs like Flexeril.
Both drugs reduce muscle contraction by lowering excitability, not by correcting the underlying cause of tension or cramping.
Flexeril works centrally by depressing neural signaling to skeletal muscle. Magnesium works peripherally by altering ionic gradients that muscles and nerves rely on to fire. Different entry points, same outcome: forced relaxation. That’s why you think it’s working to relieve your muscle cramping. It is masking the symptoms, which is why the return occurs when you stop either drug.
That relaxation feels therapeutic because symptoms quiet down. But just like Flexeril, magnesium does not restore normal mechanics or signaling. It overrides them. When the vascular muscle is relaxed this way, pressure drops, force delivery falls, and the kidneys are forced to compensate to maintain filtration. Muscle cramps resolve because contraction thresholds are chemically suppressed. That feels corrective. It is not. Magnesium does not restore normal electrical balance. It overrides excitability, causing the body to compensate.
A lower tone means a lower force is delivered to the kidneys. Filtration cannot fall, so the kidneys compensate mechanically and electrically to preserve clearance. Now the kidneys are taxed. A few days of this, your body can handle. In a few months and years, you are pushing your kidneys to the breaking point.
Cramps are often a signal of pressure instability, volume imbalance, or disrupted charge dynamics. Magnesium silences that signal by pharmacologic relaxation.
Supplements Marketed as “Heart Healthy”
This category causes real damage because it is trusted.
Nitric oxide boosters work by forcing vasodilation. Resistance drops. Pressure drops. Filtration force drops. Compensation rises.
Fish oil alters platelet behavior and vascular responsiveness. Subtle changes, repeated daily, shift how pressure is handled. Eat the whole fish, not the isolated oil that is rancid. If a supplement “improves circulation,” it is interfering with regulation. There is no exception clause for good intentions.
Cosmetic and Performance Drugs (Where the Mechanism Is Impossible to Ignore)
Minoxidil was a blood pressure drug before it was a hair product. Hair regrowth is a side effect of vasodilation. That same vasodilation reduces the force available to kidney filtration.
Hair grows. Kidneys compensate…until they don’t.
Sildenafil, Viagra, and related drugs enhance nitric oxide signaling. They lower resistance and pressure transiently. Used repeatedly, they become another chronic tone disruptor.
Improved erections do not improve kidney physiology. They are simply proof that vasodilation worked. But you borrowed from one system to pay another until the bank runs dry, and you have to start stealing from the body until it finally can no longer function on borrowed time and succumbs to your chemical insults.
HTR, Hormones and Hormone Mimics
The thyroid hormone increases heart rate and contractility. Steroids alter volume and sodium handling. Sex hormones shift vascular compliance. These are not side effects. They are pressure modifiers by design.
Changing hormones changes pressure requirements. The kidneys adapt until they can’t.
Why Solvents Always Do Damage
Solvents like DMSO, turpentine, and related compounds are effective precisely because they dissolve fats and disrupt lipid structures. That is their defining property. Myelin, cell membranes, and vascular linings are fat-rich lipid structures. When a solvent enters the bloodstream, it does not “target toxins.” It interacts with whatever lipid surfaces it encounters.
Myelin is an insulating sheath composed largely of lipids. Its function depends on structural integrity. Solvents weaken that integrity by solubilizing lipid components, altering membrane permeability, and destabilizing electrical signaling. The result is impaired nerve conduction, altered vascular tone, and increased reliance on compensatory pressure mechanisms to maintain flow and filtration.
The same chemistry applies to fatty deposits and protective lipid layers in blood vessels and kidneys. Solvents dissolve what they contact indiscriminately. When lipid barriers are disrupted, resistance increases, signaling becomes erratic, and pressure requirements rise to preserve function. It is chemical interference with structures the body depends on to regulate flow, charge, and filtration.
Solvents do exactly what they are designed to do. The problem is not that they work. The problem is what they work on.
The Rule That Has Not Failed Yet
If something:
- relaxes blood vessels
- alters volume
- changes signaling
- “improves circulation”
- suppresses a symptom without reducing load
Then it alters pressure in the kidney’s until it reaches a point of permanent damage.
The Final Checkmate
Every intervention discussed above shares the same underlying problem: it falsely alters force, charge, or volume without reducing the load that must be cleared. Blood pressure drugs, electrolyte manipulation, supplements, vasodilators, hormones, and so-called “heart-healthy” products do not remove metabolic waste, chemical burden, or resistance, they add to it. They redistribute the workload so you think the intervention is working.
The heart generates pressure. The kidneys require pressure to filter blood. When force is artificially reduced, vessels are relaxed, charge gradients are disrupted, or volume is diluted, filtration is not optional.
This progression is not mysterious. It does not require a rare disease, bad luck, or toxic intent. It follows directly from asking a closed system to perform the same work under worse conditions for years. When numbers improve while reserve disappears, the outcome is delayed, not prevented.
You cannot separate heart health from kidney health. You cannot suppress a signal and call it resolution. And you cannot repeatedly interfere (enter a state of fear so you interfere) with the mechanics of circulation without eventually losing the organs that depend on them.
That is the end of the argument. Oh and check the references. I am basing this on evidenced based reality, not industry sponsored paid for peer reviewed garbage from your practitioner who profits from your ignorance.
A Note Before You Go
I have a sincere favor to ask.
This work is increasingly being restricted, removed, or quietly buried across platforms. That includes TikTok, YouTube, and now even here. What is happening globally, including readers being locked out of accounts for refusing biometric verification while still being charged, makes one thing clear: content that exists only on platforms is not safe.
Agent131711 and I spend hours every day researching, cross-checking, writing, and preserving this material. No sponsors. No affiliates. No corporate products. Just time, costs, and a commitment to tell the truth plainly. That’s why we are building the Shadow Banned Library, a place where this work can be downloaded, stored, printed, and passed on before it disappears.
If this article mattered to you, please consider supporting that effort. Subscribing, donating, and sharing all help keep this work alive while we still can.
Important note for readers:
If you are ever locked out of your account due to platform requirements such as biometric verification, please do not file a chargeback. Chargebacks create significant banking penalties and make refunds harder, not easier and end up costing me more money than I received. If this happens, email me directly at robin@purifywithin.com, and I will cancel your subscription and refund any prepaid amount. More detailed guidance will follow in a separate email.
You can learn more about the preservation effort at shadowbannedlibrary.com.
Thank you for reading, for thinking critically, and for supporting work that refuses to be bought or softened.
Disclaimer
The views expressed in this article are the author’s opinions, based on clinical experience, historical sources, public records, and secondary reporting. Where applicable, references to peer-reviewed and archival material are provided to support discussion of physiology and public health policy.
The author is a licensed Registered Nurse (RN) no longer working in the field. This article reflects professional observation and analysis, but it is not intended as individualized medical advice, diagnosis, or treatment. Readers should consult their own licensed healthcare professionals for personal medical decisions.
This piece is written for informational and educational purposes only. It does not allege proven legal wrongdoing by any named company or individual.
If you believe this article contains a factual error, or if you represent an entity mentioned and wish to provide source documentation or request a correction, please contact robin@purifywithin.com. Corrections will be made promptly where warranted.
Nothing in this article should be construed as legal advice. For legal guidance regarding publishing, liability, or defamation, consult a qualified attorney.
References:
Kidney Filtration, Pressure, and Dialysis
Brenner, B. M., & Rector, F. C. (2008). The kidney (8th ed.). Philadelphia, PA: Saunders Elsevier.
→ Foundational nephrology text on glomerular filtration, pressure dependence, proteinuria, and progression to renal failure.
Levey, A. S., Coresh, J., Balk, E., Kausz, A. T., Levin, A., Steffes, M. W., … Eknoyan, G. (2003). National Kidney Foundation practice guidelines for chronic kidney disease. Annals of Internal Medicine, 139(2), 137–147. https://doi.org/10.7326/0003-4819-139-2-200307150-00013
→ Documents progressive kidney damage, proteinuria, and clinical markers.
Blood Pressure Lowering, Kidney Compensation, and RAAS
Guyton, A. C., Hall, J. E., & Hall, M. E. (2021). Guyton and Hall textbook of medical physiology (14th ed.). Philadelphia, PA: Elsevier.
→ Core physiology of pressure–flow relationships, renal autoregulation, and compensation.
Bidani, A. K., & Griffin, K. A. (2004). Pathophysiology of hypertensive renal damage. Hypertension, 44(5), 595–601. https://doi.org/10.1161/01.HYP.0000145181.30401.f6
→ Shows how altered pressure distribution damages renal microstructure over time.
Diuretics, Potassium Loss, and Arrhythmias
Ellison, D. H., & Felker, G. M. (2017). Diuretic treatment in heart failure. New England Journal of Medicine, 377(20), 1964–1975. https://doi.org/10.1056/NEJMra1703100
→ Mechanisms of sodium, water, and potassium loss with diuretics.
Gennari, F. J. (1998). Hypokalemia. New England Journal of Medicine, 339(7), 451–458. https://doi.org/10.1056/NEJM199808133390707
→ Links hypokalemia to arrhythmias and vascular instability.
Electrolytes, Vascular Tone, and Calcification
London, G. M., & Drüeke, T. B. (1997). Atherosclerosis and arteriosclerosis in chronic renal failure. Kidney International, 51(6), 1678–1695. https://doi.org/10.1038/ki.1997.228
→ Vascular stiffness, calcification, and increased pressure demand in kidney disease.
Giachelli, C. M. (2009). The emerging role of phosphate in vascular calcification. Kidney International, 75(9), 890–897. https://doi.org/10.1038/ki.2008.644
→ Mechanisms of mineral-driven calcification.
Vitamin D, Calcium, and Vascular Stiffness
Pilz, S., Tomaschitz, A., Drechsler, C., Dekker, J. M., & März, W. (2011). Vitamin D deficiency and myocardial diseases. Molecular Nutrition & Food Research, 54(8), 1103–1113. https://doi.org/10.1002/mnfr.201000061
→ Vitamin D as a hormone affecting vascular and renal systems.
Shroff, R., Long, D. A., & Shanahan, C. (2013). Mechanistic insights into vascular calcification in CKD. Journal of the American Society of Nephrology, 24(2), 179–189. https://doi.org/10.1681/ASN.2011121191
→ Direct link between calcium handling, calcification, and kidney damage.
Magnesium, Vasodilation, and Muscle Relaxation
Touyz, R. M. (2004). Magnesium in clinical medicine. Frontiers in Bioscience, 9, 1278–1293. https://doi.org/10.2741/1334
→ Magnesium as a smooth muscle relaxant affecting vascular tone.
Romani, A. M. (2013). Magnesium in health and disease. Metal Ions in Life Sciences, 13, 49–79. https://doi.org/10.1007/978-94-007-7500-8_3
→ Mechanisms of magnesium altering excitability and muscle contraction.
Nitric Oxide, Vasodilation, and Pressure Reduction
Ignarro, L. J. (2002). Nitric oxide as a unique signaling molecule in the vascular system. Circulation Research, 90(1), 21–28. https://doi.org/10.1161/hh0102.102978
→ Nitric oxide’s role in vasodilation and pressure reduction.
Klabunde, R. E. (2012). Cardiovascular physiology concepts (2nd ed.). Philadelphia, PA: Lippincott Williams & Wilkins.
→ Standard physiology reference for vascular resistance and flow.
Dialysis Outcomes and Progression
United States Renal Data System. (2023). USRDS annual data report: Epidemiology of kidney disease in the United States. Bethesda, MD: National Institutes of Health.
→ Epidemiology of CKD progression and dialysis dependence.
Structured Water, Charge, and Blood Flow (Electrical Component)
Pollack, G. H. (2013). The fourth phase of water: Beyond solid, liquid, and vapor. Seattle, WA: Ebner & Sons.
→ Describes structured water, charge separation, and biological flow adjacent to surfaces.
____
https://medicinegirl.substack.com/p/be-still-my-beating-kidneys?